 |
 |
| J Rhinol > Volume 30(3); 2023 |
|
Abstract
Background and Objectives
Methods
Results
Notes
Availability of Data and Material
The datasets generated or analyzed during the study are available from the corresponding author on reasonable request.
Author Contributions
Conceptualization: Shin Hyuk Yoo. Data curation: Hyo-Yeon Kim, Yoon-Ah Kim. Formal analysis: Shin Hyuk Yoo, Hyo-Yeon Kim. Funding acquisition: Shin Hyuk Yoo, Ji-Hun Mo. Investigation: Shin Hyuk Yoo, Hyo-Yeon Kim. Methodology: Shin Hyuk Yoo. Project administration: Ji-Hun Mo. Resources: Shin Hyuk Yoo, Ji-Hun Mo. Software: Hyo-Yeon Kim, Yoon-Ah Kim. Supervision: Ji-Hun Mo. Validation: Shin Hyuk Yoo, Ji-Hun Mo. Visualization: Shin Hyuk Yoo, Hyo-Yeon Kim. WritingŌĆöoriginal draft: Shin Hyuk Yoo, Hyo-Yeon Kim. WritingŌĆöreview & editing: Shin Hyuk Yoo, Ji-Hun Mo.
Funding Statement
This research was supported by the Basic Science Research Program of the National Research Foundation of Korea, funded by the Ministry of Education [2021R1I1A1A01052298]. This research was also supported by a grant from the Korea Health Technology R&D Project of the Korea Health Industry Development Institute, funded by the Ministry of Health and Welfare, Republic of Korea (grant number: HI22C0612).
This research was supported by the Bio & Medical Technology Development Program of the National Research Foundation (NRF) funded by the Korean government (MSIT) (RS-2023-00220408). This research was supported by Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Science, ICT & Future Planning (2020R1A2C1012105). This research was supported by Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Education (NRF-2020R1A6A1A03043283).
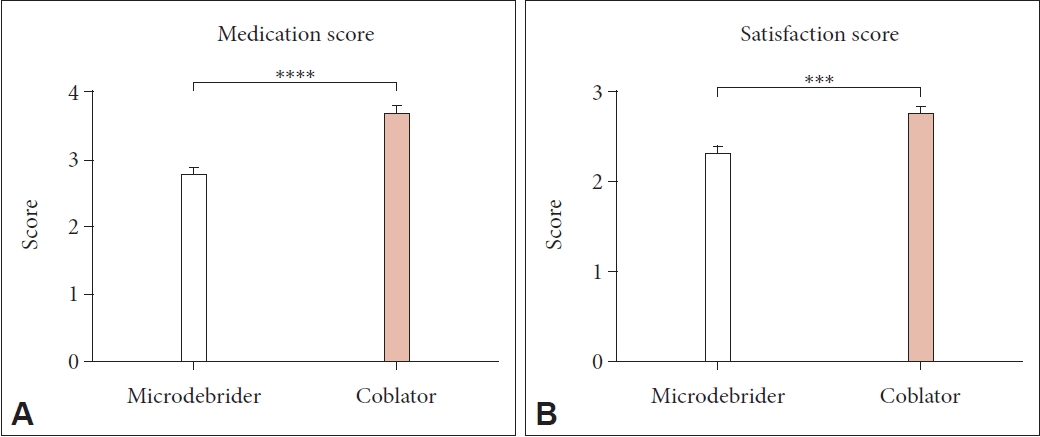
Fig.┬Ā1.

Fig.┬Ā2.

Fig.┬Ā3.
Table┬Ā1.
| Variable | Microdebrider group (n=192) | Coblator group (n=49) | p* |
|---|---|---|---|
| Male:Female | 137 (71.3):55 (28.7) | 42 (85.7):7 (14.3) | 0.0631 |
| Age (yr) | 26.4┬▒14.8 | 27.1┬▒11.7 | <0.0001 |
| Initial symptom score | |||
| ŌĆāNasal obstruction | 6.02┬▒2.93 | 6.57┬▒2.58 | 0.1812 |
| ŌĆāRhinorrhea | 5.10┬▒3.13 | 5.18┬▒3.08 | 0.7303 |
| ŌĆāSneezing | 4.25┬▒3.13 | 5.18┬▒2.86 | 0.1842 |
| ŌĆāItching | 3.52┬▒3.34 | 4.57┬▒2.92 | 0.0647 |




 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Print
Print




