Assessing Feasibility and Safety of Using Ultrasonic Bone Aspirator for Revision Endoscopic Sinus Surgery
Article information
Abstract
Background and Objectives
This study introduced and evaluated the efficacy of an ultrasonic bony aspirator (UBA) in revision endoscopic sinus surgery and compared the outcomes to those of the traditional cold instrument approach.
Methods
This retrospective study enrolled 57 patients who underwent revision endoscopic sinus surgery between June 2010 and December 2017, 17 patients with a UBA approach and 40 patients with traditional instruments.
Results
Median Lund–Kennedy scores showed a statistically significant difference between the two groups at 3 months (p=0.004). Synechiae occurred in 17.6% and 35% of cases in the UBA and traditional groups, respectively. The mean operative time was significantly shorter in the traditional group (p=0.001).
Conclusion
The use of a UBA in revision endoscopic sinus surgery was safe and effective.
INTRODUCTION
Endoscopic sinus surgery (ESS) is performed for the treatment of chronic rhinosinusitis (CRS) with or without nasal polyps refractory to pharmacological treatment, fungal sinusitis, inverted papillomas, and nasal cavity tumors. The estimated prevalence of CRS is 1.1%–19.9% in adults worldwide [1,2]. ESS is recommended when medical therapy for the management of CRS is unsuccessful, and approximately 200,000–300,000 ESSs are performed in the United States annually [3].
Despite extensive primary surgical therapy and postoperative medical therapy, up to 20% of patients who undergo sinus surgery show residual disease and require revision surgery [4-10]. Several factors can lead to the failure of primary surgery, including retained air cells in the frontal recess or anterior and posterior ethmoid; obstruction of the sphenoid ostia; remnant uncinate process leading to the recirculation phenomenon [11-13]; fibrosis and adhesion [14,15]; and osteitis or new bone formation, which may obstruct the natural ostium [16-18].
Major complications such as cerebrospinal fluid leakage, meningitis, hemorrhage, and orbital injury may occur during revision surgery [19]. Several studies have shown statically different outcomes, making the comparison between the complication rates of primary and revision surgeries controversial. However, revision surgery is more challenging for operators and more likely to result in complications [20-23]. The challenge to operators comes from decreased visualization, altered surgical landmark anatomies, bleeding, osteitis, and new bone formation [24].
Recently, with the development of medical technology, numerous surgical instruments, such as ultrasonic bone aspirator (UBAs), have been utilized for bony work. UBAs were first developed for brain surgery in neurosurgery. In these tools, ultrasonic oscillation is used to emulsify bone, avoiding mechanical and thermal damage to the surrounding tissues. The present study evaluated the availability and utility of UBA (SONOPET; Mutoh Co, Ltd, Tokyo, Japan) in revision ESS and compared the outcomes to those of the traditional cold instrument approach.
We compared the overall complication rates, postoperative endoscopic findings of healing mucosa, and operative time between patients on whom UBA was used and those on whom conventional instrumentation with traditional instruments was used to assess the feasibility of the use of this new instrument.
METHODS
Subjects
We retrospectively reviewed the data of 79 patients who underwent revision ESS by two expert rhinologists at the authors’ clinic between June 2010 and December 2017 performed. All patients had undergone ESS at least once. We excluded patients diagnosed with malignancies, benign tumors, inverted papillomas, mucoceles, and osteomas, as well as those with a short follow-up duration or incomplete medical records. The patients were divided into two groups: an experimental group who had undergone the procedure with UBA and a control group who had undergone treatment with traditional instruments (cold instruments with or without microdrills). The authors used UBA in cases of lesions close to vital structures such as the skull base, lamina papyracea, or optic nerve. Severe osteitic change on preoperative computed tomography (CT) was also an indication for UBA application. Traditional instruments were also used in some cases. The patients who underwent revision ESS were refractory to medication. The surgical extent was planned based on CT scans and nasal endoscopy. Postoperative medication was administered to prevent secondary infections and reduce inflammation. In the presence of edema or polyp changes in the healing mucosa, topical nasal spray was used.
The study protocol was approved by the Institutional Review Board (2019-01-005-003) of Kosin University Gospel Hospital.
Analytic factors
Preoperative CT scans were performed; staging using the Lund–MacKay system (LMS) [25] and sinonasal endoscopic assessment were performed and severity was graded using the Meltzer scores to classify the nasal endoscopic polyps [26] in all patients. The outcomes were determined according to the Lund–Kennedy (LK) endoscopic scoring system [27], the number of complications, the operative time, and the recurrence of nasal polyps. Postoperative LK endoscopic scores were also assessed postoperatively at 0 (1–14 days), 1 (15–30 days), 2 (31–60 days), and 3 (61–90 days) months and compared between the groups. The total operative times were compared between the groups. Postoperative complications, including bleeding, skull base injuries, orbital injuries, nasolacrimal duct injuries, and anosmia, were checked by reviewing the medical records. Symptom and polyp recurrence were also assessed.
Description of surgical procedure
Careful preoperative evaluations were performed using CT scans in all patients to determine the extent of surgery, to identify the critical structures at risk (orbit, optic nerves, cribriform plate, and nasolacrimal duct), and to determine the neoosteogenetic regions requiring the use of UBA or traditional instruments. The surgeries were performed under general anesthesia. A surgical navigation system was used intraoperatively in all patients to accurately localize the pathologic regions and overcome possible difficulties caused by altered anatomy (Fig. 1). The operator approached the sinuses in the same manner as in conventional ESS. Every conventional ESS was performed using traditional cold instruments, with or without microdrills. The UBA was utilized primarily in hyperossified regions that were refractory to traditional cold instruments (antrum punch, rongeurs, antrum curettes, blakesley forceps) (Fig. 2A) or if the circumferential structures might be affected by the microdrill burr blades.

Localization of the ethmoid hyper-ossified air cell using the navigation system before applying the ultrasonic bone aspirator
Intraoperative endoscopic finding. A: Removal of a localized hyper-ossified ethmoid air cell using an ultrasonic bone aspirator. Only the claw portion of the device is active, which enables precise and meticulous sculpting without damaging the surrounding structures. B: When using drills in sinus surgery, the surrounding mucosa may be twisted by the rotation shaft or burr.
Statistical analysis
Statistical analysis was performed using R 3.5 software (R Foundation for Statistical Computing, Vienna, Austria). When non-normally distributed data were analyzed using nonparametric methods. For all statistical tests, p<0.05 was considered significant. Differences were analyzed using chi-square tests for dichotomous data and Wilcoxon rank-sum tests to compare numeric variables between two groups.
RESULTS
Demographic factors
We enrolled 57 of 79 patients who met the study inclusion criteria, including 17 patients who had undergone ESS with UBA (experimental group) and 40 patients who had undergone ESS procedures with traditional instruments (cold instruments with or without microdrills) (control group). The average ages of the patients in the UBA and traditional groups were 46.94 and 46.28 years, with male-to-female ratios of 10:23 and 7:17, respectively. The number of prior sinus procedures in patients ranged from 1 to 3 (mean, 1.29) and 1 to 2 (mean, 1.02) in the two groups. The mean periods between the most recent sinus surgery and revision ESS procedure in the UBA and traditional groups were 269.06 months (range: 2.6–395.7 months) and 401.35 months (range: 5.39–534.8 months), respectively (Table 1).
Preoperative data
The mean LMS values were 6.35 and 4.81 in the UBA and traditional groups, respectively (range: 0–10). The average endoscopic nasal polyp grading scores were 1.91 and 1.17 (range: 0–4) and preoperative polyps were found in 11 (64.7%) and 25 (62.5%) patients in the UBA and traditional groups, respectively. The navigation system was used in 94.1% of patients in the UBA group and 35.0% of patients in the traditional group (Table 1). The mean operation time was significantly shorter in the traditional group (p=0.001; Table 1).
Postoperative data
The UBA group had median (interquartile range) LMS values of 3 (range: 1–5) preoperatively, 2 (range: 0–4) at 1 month, 1 (range: 0–3) at 2 months, and 0 (range: 0–2) at 3 months. At the same follow-up periods, the traditional group had median nasal endoscopic scores of 3 (range: 1–6), 2.75 (range: 0–5), 1 (range: 0–5), and 1 (range: 0–4). The groups differed significantly at 3 months (p=0.004, Wilcoxon rank-sum test) (Fig. 3).
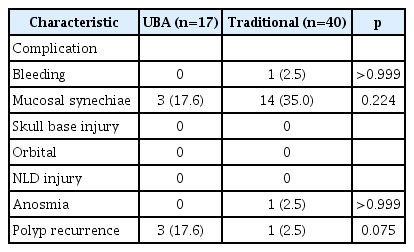
Postoperative complications
Mucosal synechiae occurred in 17.6% and 35.0% of cases in the UBA and traditional groups, respectively. Only one case of postoperative bleeding occurred in the traditional group. Nasal polyp recurrence was observed in 17.6% of cases in the UBA group and 2.5% of cases in the traditional group; however, the difference was not statistically significant (Table 2).
DISCUSSION
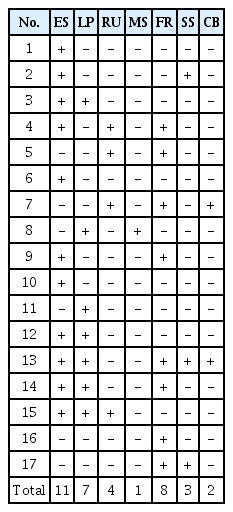
During ESS, new bone formation in the paranasal sinuses is challenging. Cho et al. [28] reported the impact of previous surgery on anterior ethmoid bone density, including significantly higher new bone formation and bone density compared to those during primary ESS. In the present study, hyperossified regions of new bone formation were found using UBA mainly in retained ethmoidal air cells (11, 30%), frontal recess (8, 22%), lamina papyracea (7, 19%), remnant uncinate process (4, 11%), and sphenoid face (3, 8%) (Table 3). Numerous types of traditional instruments have been used to remove hard bones in ESSs, including drills and cold instruments. Advantages of using drills for ESS are that various tips have been developed and can be selected according to the operator’s preference and lesion status. Also, the rotation speed of drills and the force applied by the operator to the lesion can be adjusted so that the lesion can be removed in menticulous control. However, these instruments have limitations in removing hyper-ossified bone proximal to vital paranasal sinus structures, such as the orbit, optic nerves, cribriform plate, and arteries, due to increased risk to the surrounding structures, as these instruments do not exert enough force to manipulate the hard bone. Also, drills can make high temperature and soft tissue damage that could result in some complications such as mucosal synechiae. Several studies have demonstrated good outcomes from ESS performed using UBA [29,30]. The UBA is comparable to traditional drills in ESS in power while allowing the operator to perform more precise, meticulous, and safe bone sculpting during ESS.
Drills have rotating 360° blades that can circumferentially damage unwanted structures (Fig. 2B). In contrast, UBA uses only a unilateral surface to remove the bone; this directionality offers potential benefits in protecting the contra-lateral structures from damage, including vital structures such as the optic nerve or carotid artery, when widening the sphenoid natural ostium, ethmoid artery, lamina papyracea, or cribriform plate when widening the frontal recess.
In cases requiring widening of the frontal recess, the straight UBA tip has a limited approach and cannot access the uppermost portion of the frontal recess. Although currently lacking, an angulated tip suitable for frontal sinus surgery existed would be a useful and safe feature of this instrument. Massey et al. also reported the need for the optimization of frontal sinus-specific angulation for the UBA for frontal applications. The combined use of the UBA and curved microdrills for frontal recess surgery might be the best approach at this point.
The UBA can remove bone continually and efficiently. Studies have shown that UBAs induce less damage to the surrounding soft tissue [30]; thus, UBAs reduce damage to the surrounding nasal mucosa and reduce the risk of postoperative mucosal synechiae (Fig. 4).
Postoperative endoscopic view of left ethmoid cavity using ultrasonic bone aspirator. A: After 1 week. B: After 4 weeks. C: After 10 weeks.
Appropriate bone removal when using drills requires the operator to apply force on both the instrument and the structure being removed. However, with UBAs, excessive force is not required to remove the bones; only the slight contact of the claw with the bone is sufficient for sculpting [29]. The UBA can even sculpt mobile bone fragments, which may minimize cracking or fracture of the lamina papyracea or ethmoid roof during manipulation. Furthermore, unlike drills, UBAs do not have kick-back or uncontrolled movements, thus reducing potential injury to the surrounding structures. UBAs also have concurrent suction and irrigation to enhance the visual field of surgery and reduce heat-related injuries. Moreover, these instruments do not produce bone dust, unlike drills, which also improves the visual field. Overall, multiple factors indicate that the operator can manipulate and sculpt structures exactly, safely, and precisely using the UBA, in the required locations. Considering these characteristics, UBAs may reduce the risk of postoperative complications.
Although the difference was not statistically significant, nasal polyp recurrence was higher in the UBA group in the present study. This could be explained by the UBA indications in this study, in which UBA was applied in more severe cases, such as those with high risks of injury to vital structures during surgery or severe osteitic changes on previous CT scans. This could explain the higher recurrence of nasal polyps.
Reduced heat injury implies less damage to the surrounding mucosa or low chances of bone injury that could result in “crusting and scaring (adhesion)” in the LK endoscopic scoring system. However, our study did not show any statistically significant differences between the UBA and traditional groups of patients. Therefore, prospective studies are required to compare heating damage and subsequent complications.
While several studies have demonstrated a reduced operative time for dissection with UBA, in the present study, the average operative time differed significantly, favoring conventional instrumentation. This discordance may be due to more complicated cases using UBA, with a higher preoperative LMS compared to those cases using conventional instrumentation. Indeed, the drills can remove a large amount of bones at once using tips of various diameters, whereas UBA can use limited types of tips for neurosurgery, so it is difficult to remove many lesions at once. That may had been resulting in more operation time of UBA groups. However, the subjective convenience of usage was better with UBA.
UBA seems to be safe and effective in revision ESS, avoiding injury to the vital structures. However, UBA tips with an angled design are needed to reach the uppermost portion of the frontal recess and effectively widen the hypertrophied bones around the frontal recess. In conclusion, UBA may be considered a suitable option with added benefits in revision ESS.
Notes
Availability of Data and Material
All data generated or analyzed during the study are included in this published article.
Conflicts of Interest
The authors have no potential conflicts of interest to disclose.
Author Contributions
Conceptualization: Jae Hwan Kwon. Data curation: Joo Yeon Kim. Formal analysis: Joo Yeon Kim, Jung Ho Oh. Methodology: Seo Bin Kim. Supervision: Jae Hwan Kwon. Validation: Joo Yeon Kim. Visualization: Seo Bin Kim. Writing—original draft: Jae Hwan Kwon. Writing—review & editing: Joo Yeon Kim.
Funding Statement
None