 |
 |
| J Rhinol > Volume 30(3); 2023 |
|
Abstract
Background and Objectives
This study aimed to elucidate the relationship between nasal septal deviation (NSD) and upper lateral cartilage (ULC) collapse.
Methods
We conducted a retrospective review of 142 paranasal sinus computed tomography scans from patients who had undergone septoplasty due to confirmed NSD. The ULC angle was measured on both the narrow and wide sides of the nasal cavities, and these measurements were compared to evaluate the extent of ULC collapse in relation to the degree of NSD and patient age. The correlation between the degree of NSD and the degree of ULC collapse was also analyzed.
Results
The mean ULC angle was found to be 13.4┬░┬▒2.7┬░ on the narrow side and 14.3┬░┬▒2.7┬░ on the wide side, with a statistically significant difference between the two (p<0.001). When comparing caudal and non-caudal NSD patients, there was no significant difference in the degree of ULC on either side (p=0.166). When comparing the ULC angle between two age groups (Ōēź50 vs. <50 years), the difference in ULC angles was significantly greater in the group of patients aged under 50 years (0.3┬░┬▒3.8┬░ vs. 1.1┬░┬▒2.2┬░, p=0.014). There was a significant positive correlation between the degree of ULC collapse and the degree of septal deviation (r=0.214, p=0.01).
Nasal airway obstruction, which is a condition with a multifactorial etiology, significantly affects patientsŌĆÖ quality of life [1]. Anatomic contributors to nasal airway obstruction include nasal septal deviation (NSD), an enlarged inferior turbinate, and static or dynamic nasal valve dysfunction [2]. Among the numerous structures of the nasal airway, the nasal valve is the narrowest portion of the human airway [3]. Resistance of the nasal airway accounts for more than 50% of the total airway resistance, most of which occurs in the nasal valve [4-6]. Consequently, even minor changes in the size of the nasal valve can significantly alter airflow resistance, which in turn affects nasal function [7-9]. The nasal valve region is composed of three structures: the inferior turbinate, the nasal septum, and the lateral nasal wall. The external nasal valve is formed medially by the caudal septum and columella, superiorly by the weak triangle, laterally by the alar rim, and inferiorly by the floor of the nasal vestibule [10].
The internal nasal valve (INV) is anatomically formed by the caudal border of the upper lateral cartilage (ULC), the nasal septum, the head of the inferior turbinate, and tissues surrounding the pyriform aperture. Therefore, it is important to identify which of these structures may be negatively impacting the function of the nasal valve. The integrity of INV structures can be compromised due to nasal aging, traumatic injury, or previous nasal surgery [11]. In patients with nasal obstruction, it is essential to assess the nasal valve, because nasal valve dysfunction is as common as septal deviation and an enlarged inferior turbinate [12-14].
As the ULC is one of the structures establishing the INV, collapse of the ULC can result in nasal obstruction. Unlike the nasal septum and inferior turbinate, which are static and rigid, the ULC is less rigid, making it a variable determinant for nasal valve stability [15]. BernoulliŌĆÖs principle states that as the speed of a moving fluid (either liquid or gas) increases, the pressure within the fluid decreases [16]. Consequently, it can be inferred that the airflow rate in the nasal cavity on the same side as the septal deviation is higher than that in the opposite nasal cavity. This could result in repetitive pressure being applied to the ULC on the side of the septal deviation. We propose that the force exerted by this negative pressure could cause the ULC to collapse statically, leading to increased obstruction of the nasal airway. However, several other factors could influence the development of nasal valve stenosis, such as trauma. Our hypotheses would be further substantiated if the aforementioned computational fluid dynamics analysis is conducted in a future study.
To date, no studies have investigated the relationship between NSD and ULC collapse. Therefore, the aim of this study was to explore the association between NSD and ULC collapse using computed tomography (CT) images.
We analyzed CT scans of the paranasal sinus (PNS) from a consecutive series of 142 patients. These patients visited the Otolaryngology Department of Asan Medical Center between October 2017 and May 2019, presenting with complaints of nasal obstruction. Each patient had been diagnosed with a deviated nasal septum and had undergone septal surgery. All subjects enrolled in the study were at least 18 years old and had undergone a physical examination during their outpatient clinic visit. In these patients, dynamic INV collapse was ruled out as a diagnosis by evaluating INV collapse during forced inspiration. This study did not include CT scans showing the PNS of patients with acute or chronic rhinosinusitis, nasal polyps, maxillofacial fractures, and/or a history of sinonasal surgery.
The scans were acquired using multislice CT machines (scan settings: 120 kV and 200 mA; SOMATOM Definition AS+; Siemens Healthcare GmbH, Erlangen, Forcheim, Germany). Each scan was conducted with 2.5-mm-thick sections, in both the axial and coronal planes.
We assessed the collapse of the ULC at the level of the INV by measuring the ULC angle, between the most protruding part of the ULC and the facial midline, with the INV being one cut anterior to the most anterior part of the inferior turbinate [17]. To eliminate the influence of NSD, we established the facial midline using the anterior nasal spine and crista galli as reference points. We then measured the ULC angles on the left and right sides separately. Using these same reference points, we also assessed the degree of NSD. The gap in the ULC angle between the two sides of the nasal cavity was estimated to evaluate the extent of ULC collapse (Fig. 1A). The ULC angle was measured on the narrow (a) and wide (b) sides from the most protruding part of the ULC to the facial midline (from the nasion to the anterior nasal spine). If the ULC angle on the wide side is larger than that on the narrow side, the gap value was deemed positive, while it was considered negative in the converse case. The degree of septal deviation was estimated (c) by comparing the line from the premaxilla to the crista galli with the line from the crista galli to the most prominent point of the nasal septum on the narrow side of the nasal cavity (Fig. 1B) [18].
Subgroup analyses were also carried out to further validate the association between caudal septal deviation or age and ULC collapse. NSD was classified as a caudal septal deviation when it was anterior to the anterior nasal spine [19].
All analyses were performed using the independent sample t-test and Pearson correlation test in SPSS software (version 22.0; IBM Corp., Armonk, NY, USA). A p-value of <0.05 was considered to indicate statistical significance. A Pearson correlation coefficient (r) closer to +1 or -1 indicates a stronger association between ranks.
This study was approved by the Institutional Review Board of Asan Medical Center, University of Ulsan College of Medicine (IRB No. 2019-0948). The patientŌĆÖs consent was waived by the IRB approval.
The demographic and clinical characteristics of the patients involved in this study are outlined in Table 1. The study comprised 113 male patients and 29 female patients, with a mean age of 35.9 years (ranging from 18 to 79 years). There were 30 patients who were 50 years old or older. Among the 142 patients in this study, 57 had a deviated caudal nasal septum only. There were 48 patients with right-sided NSD and 94 with left-sided NSD. The average ULC angle on the deviated and contralateral sides was 13.4┬░┬▒2.7┬░ and 14.3┬░┬▒2.7┬░, respectively. The paired t-test revealed statistically significant differences in the ULC angle between the deviated and contralateral sides (p<0.001). The mean ULC angle gap was 0.89┬░┬▒2.66┬░. Despite the predominance of male patients in this study, there were no statistically significant differences between the male and female groups regarding the severity of septal deviation and ULC.
We compared the degree of ULC and its collapse among various subgroups (Table 2). Interestingly, there was no significant difference in ULC angles on the deviated contralateral side among patients with caudal NSD. However, patients with non-caudal NSD exhibited a statistically significant difference. A comparative analysis between the caudal septal deviation and non-caudal deviation groups showed that the difference in their ULC angles was not statistically significant (0.5┬░┬▒3.1┬░ vs. 1.1┬░┬▒2.3┬░, p=0.166). However, when comparing the degree of ULC collapse between two age groups (Ōēź50 vs. <50 years), the difference in ULC angles was significantly higher in the group consisting of patients aged less than 50 years (0.3┬░┬▒3.8┬░ vs. 1.1┬░┬▒2.2┬░, p=0.014).
The degree of ULC collapse in each patient (r=0.214, p=0.01) showed a positive correlation with the extent of NSD (Fig. 2). This statistical result suggests that the severity of ULC collapse is associated with the degree of septal deviation.
In this study, we analyzed the correlation between the degree of NSD and the collapse of the ULC using CT scans. Our findings revealed a direct correlation between the angle of NSD and the degree of ULC collapse. In addition to the deviation of the nasal septum, the collapse of the ULC itself further obstructed the nasal airway. These results imply that physicians should assess the INV prior to treating patients with NSD. Interestingly, we found no correlation between caudal septal deviation and ULC collapse.
We suggest that the results of our study can be explained by BernoulliŌĆÖs principle. The relationship between the airflow characteristics of both nasal cavities and NSD remains unestablished. Nonetheless, several researchers have explored the connection between septal deviation and airflow characteristics using computational fluid dynamics. Their studies revealed higher airflow rates and pressure in the narrower side of the nasal cavity [20,21]. The deviated septum can trigger an increase in the airflow rate, which subsequently generates a negative pressure on the ipsilateral side, leading to the collapse of the ULC. Given that ULC weakening is a symptom of aging, we hypothesized that older subjects would be more prone to ULC collapse on the deviated side. However, this group surprisingly exhibited equal degrees of ULC on both the deviated and contralateral sides. We speculate that age-related impairment of the structural stability of the ULC could result in ULC collapse on both the narrow and wide sides, irrespective of septal deviation. Since the caudal septum forms the external nasal valve, our study found no correlation between ULC collapse and caudal septal deviation.
Several previous studies have investigated the relationships between NSD, the septal body, and the enlargement of the inferior turbinate. Setlur and Goyal [18] conducted an analysis of 100 sinus CT images from patients with septal deviation, finding that the septal body tended to be more pronounced on the side opposite to the deviation. The enlargement of the inferior turbinate, seen as a compensatory response to septal deviation, has been documented in several earlier studies [22,23]. In a recent study, Yu et al. [24] found a positive correlation between septal body hyperplasia and inferior turbinate enlargement, and a negative correlation between INV area and septal body thickness. However, no previous study has explored the relationship between septal deviation and ULC collapse. To the best of our knowledge, our study is the first to investigate the correlation between NSD and ULC collapse. This study confirmed that patients with NSD are more likely to experience nasal valve collapse, with the severity of the collapse increasing with age. For patients undergoing surgery for NSD, it is crucial to determine the angle of the nasal valve. If necessary, concurrent nasal valve surgery can help alleviate the patientŌĆÖs symptoms.
The present study had some limitations. Although males generally outnumber females among patients with NSD, the male proportion in this study was notably high, which could be seen as a limitation. However, when we analyzed the data by sex, we found no statistically significant difference between the two groups. The ULC is a dynamic structure that can collapse during inhalation. Therefore, the relationship between NSD and ULC collapse warrants further evaluation, as do changes in the ULC angle during respiration. In this study, we excluded all patients diagnosed with dynamic nasal valve collapse and evaluated the ULC angle using CT imaging to assess static ULC collapse, rather than dynamic collapse. Furthermore, because this study focused solely on the analysis of radiographic parameters, it is challenging to draw strong conclusions about the clinical implications of our findings. Future research could strengthen our findings by analyzing the correlation between ULC collapse and patient symptoms, as well as airflow characteristics, which can be measured with computational fluid dynamics. A study involving acoustic rhinometry could also provide a more precise confirmation of our hypothesis. While the degree of septal deviation among the patients in this study varied (from 0┬░ to 21┬░), our study lacked a ŌĆ£negative controlŌĆØ group without any symptoms. Therefore, additional research that includes asymptomatic patients seems necessary. To further assess the impact of ULC collapse on patients with nasal airway obstruction, a prospective study comparing the postoperative results of septoplasty and nasal valve surgery with concurrent septoplasty is also recommended.
In conclusion, the degree of ULC collapse is notably linked with the degree of NSD on the convex side, which results in a more stenotic INV. These findings imply that physicians should investigate for additional concurrent anatomical abnormalities of the INV, such as ULC collapse, in patients who have a deviated nasal septum.
Notes
Availability of Data and Material
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
Author Contributions
Conceptualization: Myeong Sang Yu. Data curation: Shin Hyuk Yoo. Formal analysis: Shin Hyuk Yoo. Investigation: Shin Hyuk Yoo, Myeong Sang Yu. Methodology: Myeong Sang Yu. Project administration: Shin Hyuk Yoo, Myeong Sang Yu. Resources: Shin Hyuk Yoo, Myeong Sang Yu. Software: Shin Hyuk Yoo, Myeong Sang Yu. Supervision: Shin Hyuk Yoo, Myeong Sang Yu. Validation: Shin Hyuk Yoo, Myeong Sang Yu. Visualization: Shin Hyuk Yoo. WritingŌĆöoriginal draft: Shin Hyuk Yoo. WritingŌĆöreview & editing: Myeong Sang Yu.
Fig.┬Ā1.
Coronal computed tomography (CT) image showing the technique for measuring the degree of upper lateral cartilage (ULC) collapse (A) and septal deviation (B). The midline of the face was set with the anterior nasal spine and crista galli as reference points, and then the left and right ULC angles were measured respectively. Based on these reference points, the degree of nasal septal deviation was also evaluated.
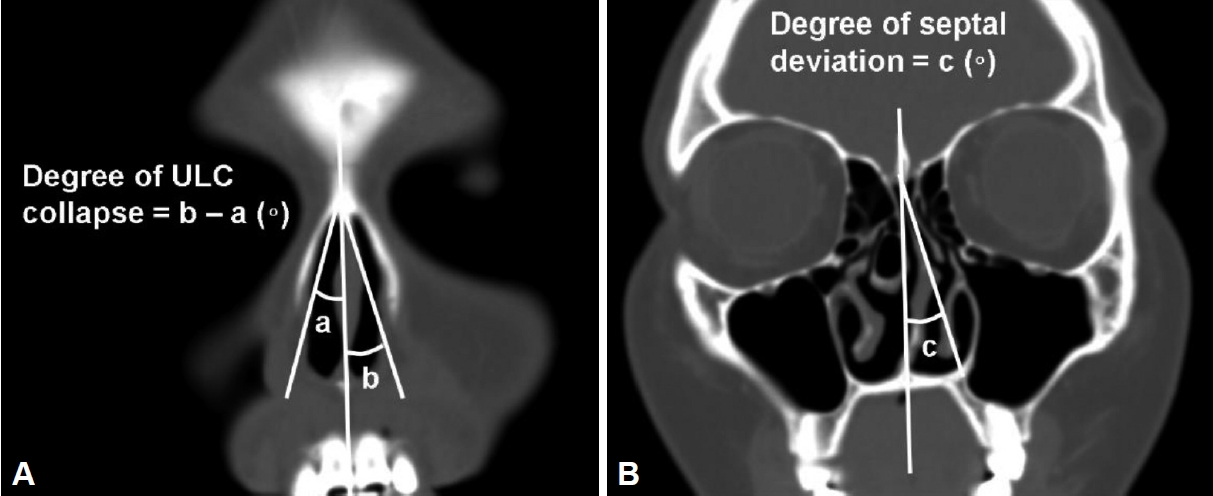
Fig.┬Ā2.
Correlation between the degree of nasal septal deviation and the degree of upper lateral cartilage (ULC) collapse.

Table┬Ā1.
Demographic and clinical characteristics of the study patients
| Variable | Value (n=142) |
|---|---|
| Mean age (range), yr | 35.9 (18ŌĆō79) |
| Sex | |
| ŌĆāMale | 113 (79.6) |
| ŌĆāFemale | 29 (20.4) |
| Deviated side of nasal septum | |
| ŌĆāRight | 48 (33.8) |
| ŌĆāLeft | 94 (66.2) |
| Degree of ULC angle (┬░)* | |
| ŌĆāDeviated side | 13.4┬▒2.7 |
| ŌĆāContralateral side | 14.3┬▒2.7 |
Table┬Ā2.
Comparison of the degree of ULC collapse between caudal septal deviation versus non-caudal septal deviation group and between the two age groups (Ōēź50 vs. <50 years)
|
ULC angle (┬░) |
ULC collapse (┬░) | p* | ||
|---|---|---|---|---|
| Deviated side | Non-deviated side | |||
| Caudal septal deviation | 0.166 | |||
| ŌĆāCaudal (n=57) | 13.3┬▒2.8 | 13.8┬▒2.7 | 0.5┬▒3.1 | |
| ŌĆāNon-caudal (n=85) | 13.4┬▒2.7 | 14.6┬▒2.7 | 1.1┬▒2.3 | |
| Age (yr) | 0.014 | |||
| ŌĆāŌēź50 (n=30) | 15.0┬▒2.8 | 15.3┬▒3.1 | 0.3┬▒3.8 | |
| ŌĆā<50 (n=112) | 13.0┬▒2.5 | 14.0┬▒2.6 | 1.1┬▒2.2 | |
References
1) Fuller JC, Levesque PA, Lindsay RW. Assessment of the EuroQol 5-dimension questionnaire for detection of clinically significant global health-related quality-of-life improvement following functional septorhinoplasty. JAMA Facial Plast Surg 2017;19(2):95ŌĆō100.


2) Barrett DM, Casanueva FJ, Cook TA. Management of the nasal valve. Facial Plast Surg Clin North Am 2016;24(3):219ŌĆō34.


4) Nigro CE, Nigro JF, Mion O, Mello JF Jr. Nasal valve: anatomy and physiology. Braz J Otorhinolaryngol 2009;75(2):305ŌĆō10.


5) Wittkopf M, Wittkopf J, Ries WR. The diagnosis and treatment of nasal valve collapse. Curr Opin Otolaryngol Head Neck Surg 2008;16(1):10ŌĆō3.


6) Bailey BJ. Head and neck surgery: otolaryngology. 2nd ed; Philadelphia, PA: Lippincott Williams & Wilkins; 1998.
7) Lee J, White WM, Constantinides M. Surgical and nonsurgical treatments of the nasal valves. Otolaryngol Clin North Am 2009;42(3):495ŌĆō511.


8) Miman MC, Delikta┼¤ H, Ozturan O, Toplu Y, Akar├¦ay M. Internal nasal valve: revisited with objective facts. Otolaryngol Head Neck Surg 2006;134(1):41ŌĆō7.



9) Cole P, Chaban R, Naito K, Oprysk D. The obstructive nasal septum. Effect of simulated deviations on nasal airflow resistance. Arch Otolaryngol Head Neck Surg 1988;114(4):410ŌĆō2.


11) Khosh MM, Jen A, Honrado C, Pearlman SJ. Nasal valve reconstruction: experience in 53 consecutive patients. Arch Facial Plast Surg 2004;6(3):167ŌĆō71.

12) Rhee JS, Weaver EM, Park SS, Baker SR, Hilger PA, Kriet JD, et al. Clinical consensus statement: diagnosis and management of nasal valve compromise. Otolaryngol Head Neck Surg 2010;143(1):48ŌĆō59.




13) Aksoy F, Veyseller B, Yildirim YS, Acar H, Demirhan H, Ozturan O. Role of nasal muscles in nasal valve collapse. Otolaryngol Head Neck Surg 2010;142(3):365ŌĆō9.



14) Clark DW, Del Signore AG, Raithatha R, Senior BA. Nasal airway obstruction: prevalence and anatomic contributors. Ear Nose Throat J 2018;97(6):173ŌĆō6.



15) Most SP. Comparing methods for repair of the external valve: one more step toward a unified view of lateral wall insufficiency. JAMA Facial Plast Surg 2015;17(5):345ŌĆō6.


16) OŌĆÖNeill G, Tolley NS. Theoretical considerations of nasal airflow mechanics and surgical implications. Clin Otolaryngol Allied Sci 1988;13(4):273ŌĆō7.


17) Bloom JD, Sridharan S, Hagiwara M, Babb JS, White WM, Constantinides M. Reformatted computed tomography to assess the internal nasal valve and association with physical examination. Arch Facial Plast Surg 2012;14(5):331ŌĆō5.


18) Setlur J, Goyal P. Relationship between septal body size and septal deviation. Am J Rhinol Allergy 2011;25(6):397ŌĆō400.



19) Wiederkehr I, Kawabata Y, Tsumiyama S, Hosokawa Y, Iimura J, Otori N, et al. Caudal septal deviation: a computed tomography-based evaluation method. Ann Plast Surg 2022;89(1):95ŌĆō9.


20) Chen XB, Lee HP, Chong VF, Wang de Y. Assessment of septal deviation effects on nasal air flow: a computational fluid dynamics model. Laryngoscope 2009;119(9):1730ŌĆō6.



21) Li L, Zang H, Han D, London NR Jr. Impact of varying types of nasal septal deviation on nasal airflow pattern and warming function: a computational fluid dynamics analysis. Ear Nose Throat J 2021;100(6):NP283ŌĆō9.



22) Berger G, Hammel I, Berger R, Avraham S, Ophir D. Histopathology of the inferior turbinate with compensatory hypertrophy in patients with deviated nasal septum. Laryngoscope 2000;110(12):2100ŌĆō5.






 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Print
Print




