 |
 |
| J Rhinol > Volume 28(3); 2021 |
|
Abstract
Nasal septal perforation (NSP) is a common complication of nasal surgery and can cause nasal obstruction, crust, and epistaxis. Many surgical methods have been introduced for repair of NSP, among which mucosal flap and artificial dermis have been widely used. However, mucosal graft can shrink and migrate and is difficult to fix at the perforation site. Mucosal advancement flap requires a wide extent of septal mucosa dissection, and artificial dermis can cause nasal obstruction because of its bulkiness and lower biocompatibility than autologous mucosa. To overcome these problems, we reported successful outcomes in 4 cases of small NSP by free mucosal graft with bioscaffold.
There are many causes of nasal septal perforation (NSP) including nasal surgery, trauma, cauterization, nasal packing, vasculitis, and nasal drug abuse [1]. Infectious and inflammatory processes, such as WegenerŌĆÖs granulomatosis, collagen vascular disease, tuberculosis and syphilis could also cause NSP [1]. Among them, nasal surgery including septoplasty and rhinoplasty is the most common cause of NSP [2]. It is associated with nasal obstruction, crusting, rhinorrhea, recurrent epistaxis, whistling sound, parosmia, and neuralgia which result in poor quality of life.
NSP is formed when both side mucoperichondriums of nasal septum are loss and blood supply is disrupted [1]. Therefore, condition of mucosa, cartilage, and blood supply of nasal cavity should be considered when repair of NSP. Various surgical techniques have been introduced to repair the NSP depending on the size of perforation and condition of mucosa and cartilage.
Small (less than 0.5 cm) and medium size (0.5 to 2 cm) defects could be closed endonasally by free mucosal graft or advancement flap with or without interposition graft including autologous and allograft [3]. Inferior turbinate free mucosal graft demonstrated satisfiable results with a success rate between 83% and 88% in case of small perforation [4,5], but it is difficult to fix to the correct perforation site and its bulk could cause nasal obstruction [4,6]. Mucosal advance flap usually requires the wide dissection extent of septal mucosa which could result in delayed healing and time spending. Rotational mucosal flap with inferior turbinate is the most popular and effective technique for small to medium size perforation [6], but symptomatic perforations usually too anterior to reach the inferior turbinate rotational flap. In addition, inferior turbinate rotational flap could cause intranasal adhesions between the septum and turbinate and nasal obstruction due to flap bulk [7]. To overcome those disadvantages, we tried to perform the turbinate free mucosal graft with bioscaffold (Lyoplant®, lyophilized bovine pericardium, type I collagen). We reported the 4 cases of small NSP repair by free mucosal graft with Lyoplant® scaffold and demonstrated successful outcomes with reduction of surgery time without complication.
We retrospectively analyzed 4 patients with NSP (<1 cm) who were repaired by turbinate free mucosal graft with Lyoplant scaffold®. After surgery, we educated the patients to perform self-irrigation of nasal cavity twice a day until 1 month, and all patients were observed every 2 weeks after surgery until 3 months. At each visit, we performed endoscopic examination and cleaned the nasal cavity.
We performed the surgery through endonasal route using endoscopy under general anesthesia, and 2% Xylocaine was infiltrated in nasal septum. Mucosa at the perforation margin was trimmed with # 12 blade and bilateral subperichondrial flaps were elevated using hemitransfixion incision at the caudal end of nasal septum. Revision septoplasty was performed (Case No. 1ŌĆō3) based on endoscopic finding and symptoms. Inferior turbinate mucosa (Case No. 2ŌĆō4) was usually harvested about 1 cm diameter, but middle turbinate mucosa (Case No. 1) was harvested when inferior turbinate mucosa showed fibrotic change due to previous turbinate surgery or severe inflammation. Lyoplant┬« was cut to 2 mm diameter larger than the perforation size, and the turbinate mucosa was fixed to the one side of the Lyoplant┬« to reduce the bulkiness of the graft using 2 stitches of Vicryl 4-0. When fixing the mucosa to the Lyoplant┬«, we spread the mucosa on the Lyoplant┬« as flat as possible to prevent shrinkage or bulkiness.
Mucosa sutured lyoplant® was laid in all direction between both side of septal mucosa at the perforation site. We placed the mucosal aspect of the bioscaffold graft to the larger perforation side or unhealthy side after subperichondrial flap elevation. The incision was repaired with vicryl 4-0, and silastic endonasal splints (silastic sheet) were placed both side of nasal septum (Figs. 1 and 2). Absorbable nasal packing was kept until 2 days after surgery, and silastic splints were removed 2 weeks after surgery.
Case No. 1 was 61 years old male who had septoplasty 3 years ago, but he had suffered from bilateral nasal obstruction and crusting which did not improve with medication. In endoscopic examination, he had right side septal cartilage deviation, left side maxillary crest protrusion, and 3 mm size perforation at 3 cm behind nostril (Fig. 3A-C).
Case No. 2 was 22 years old male who received septoplasty 6 years ago, and he had complained of left nasal obstruction from 2 years ago. Nasal endoscopic examination revealed the left side nasal septal deviation and 3 mm size perforation at 3 cm behind nostril (Fig. 3D-F).
Case No. 3 was 49 years old male who underwent septoplasty before 10 years. He had complained of sustained bilateral nasal obstruction and intermittent epistaxis. Nasal endoscopic examination showed 8 mm diameter septal perforation at caudal end of cartilaginous septum (Fig. 3G-I).
Case No. 4 was 67 years old male who received septoplasty before 30 years. He had complained of bilateral nasal obstruction and crusting. NSP of 6 mm size was observed at the caudal end of cartilaginous septum (Fig. 3J-L).
All patients were observed every 2 weeks at the outpatient clinic until complete recovery of nasal cavity mucosa. Mucosalization was completed on both sides of nasal septum without donor site complication at 1 month after surgery in all patients. Nasal symptoms were also disappeared 1 month after surgery, and no nasal discomfort and no abnormality at surgical site was observed at 3 months postoperatively.
Nasal surgery including septoplasty and rhinoplasty is commonly performed surgery to reduce nasal symptoms and improve cosmetic problems, but they could make surgical complication such as NSP. It could cause whistling sound, nasal obstruction, crusting and bleeding which might undermine quality of life. Thus, effective reconstruction technique for NSP repair is necessary to recover those symptoms.
The repair of NSP by free mucosa graft with bioscaffold demonstrated several advantages. First, it is technically easy and could save the operation time. Second, it reduced the extent of septal mucosa dissection in comparison with mucosal advance flap or septal cartilage interposition graft. Third, it did not cause nasal obstruction by repaired NSP because it is similar in thickness to the normal nasal septum. In addition, the mucosa of patients and very thin bioscaffold were used, so it could be more biocompatible than artificial dermis.
The degree of difficulty of NSP surgery depends on the size and location of the perforation. However, the classification according to the size of the perforation has not been established [3]. In general, many previous studies classified the perforation into small (less than 0.5 cm), medium (0.5ŌĆō2 cm), and large (larger than 3 cm) [8]. Large defects could be repaired by extensive flaps including facial artery myomucosal flaps, inferior turbinate pedicled flap and free flap [9,10]. Otherwise, small-to-moderate perforations could be repaired via endonasal route by mucosal graft, local advancement flaps or combined with interposition of grafts including autologous cartilage and allograft [1,11]. In this study, we focused on the patients with small to medium size (maximum 8 mm size) NSP, and we intended to perform the NSP repair more faster and easier with higher success rate without complications. However, we could not prove the efficacy of our surgical method for NSP larger than 8 mm. We did not apply this method for larger NSP because we assumed that it was difficult to fix the bioscaffold in a larger NSP and free mucosal graft could be hard to survive.
In small to moderate septal perforation, various flap methods have been introduced and the inferior turbinate rotational flap (pedicled flap) was frequently chosen for repair of NSP. Inferior turbinate rotational flap has enough blood supply and soft tissue with mucous producing ciliary nasal mucosa, but it revealed high failure rates and nasal obstruction due to flap bulkiness [3,12]. Therefore, in case of small to moderate perforation, mucosal graft and interposition graft with various graft materials have been commonly performed. The dermal allograft is biocompatible and thicker than mucosa and easier to handle than autologous fascia and commercially available, thus surgeons could save the operation time without donor site morbidity [13]. This interposition grafts provide a template for mucosa migration during the healing of perforation site after surgery and prevention of mucosa graft shrinkage and detachment. Otherwise, another previous study supported that mucosal flap combined with interposition graft showed statistically significant higher success rate than only mucosa graft [11]. Therefore, in our study, we perform mucosal graft with biocompatible bioscaffold (Lyoplant®).
The Lyoplant® is a biocompatible mesh which is acellular and avascular type I collagen derived from bovine pericardium. It has been widely used in neurosurgery for reconstructing dura defects and even in urinary bladder augmentation [14]. According to previous studies, it has several advantages for tissue regeneration and bioscaffold which are biocompatibility, absorbability, mechanical stability in order to guarantee the consistency even under abdominal pressure, support of regeneration and cell proliferation [15]. In addition, previous animal study demonstrated that Lyoplant® had sustained support for 5 weeks and cell regeneration achieved around Lyoplant® [14]. Thus, we chose Lyoplant® as bioscaffold material to reconstruct NSP, and we could not experience complication associated with this material.
Our technique of turbinate mucosa graft with Lyoplant® bioscaffold could offer several advantages. It is not as technically challenging and could make shorter surgery time. In addition, mucosa sutured Lyoplant® bioscaffold could prevent mucosa graft from escaping and shrinkage. Since the mucosa graft is spread and fixed to the Lyoplant® as much as possible, nasal obstruction due to abundant tissue could be prevented, and it is easy to fix on the correct perforation site.
In conclusion, turbinate mucosa sutured Lyoplant® bioscaffold is the effective methods for the repair of NSP in selected patients. It provides easier surgical technique without complication.
Notes
Author Contributions
Conceptualization: Nayeon Choi, Jae Hyuk Choi, Jeong Hong Kim. Data curation: Hee Jun Yi, Jaeyeop Sim, Nayeon Choi. Formal analysis: Hee Jun Yi, Jae Hyuk Choi, Nayeon Choi. Methodology: Hee Jun Yi, Jae Hyuk Choi, Nayeon Choi, Jeong Hong Kim. Project administration: Jeong Hong Kim. Visualization: Nayeon Choi, Jeong Hong Kim. WritingŌĆöoriginal draft: Hee Jun Yi, Jaeyeop Sim, Nayeon Choi, Jeong Hong Kim. WritingŌĆöreview & editing: Nayeon Choi, Jae Hyuk Choi, Jeong Hong Kim.
Fig.┬Ā1.
Endonasal repair of NSP. A: 3 mm sized NSP at caudal end of cartilaginous septum. B: Harvest of nasal mucosa from middle turbinate. C: Fixation of mucosa at the Lyoplant® scaffold. D: Subperichondrial flap elevation and placement of free mucosal graft with bioscaffold. E, F: Endoscopic view of bilateral nasal cavity after the end of NSP repair. NSP, nasal septal perforation.
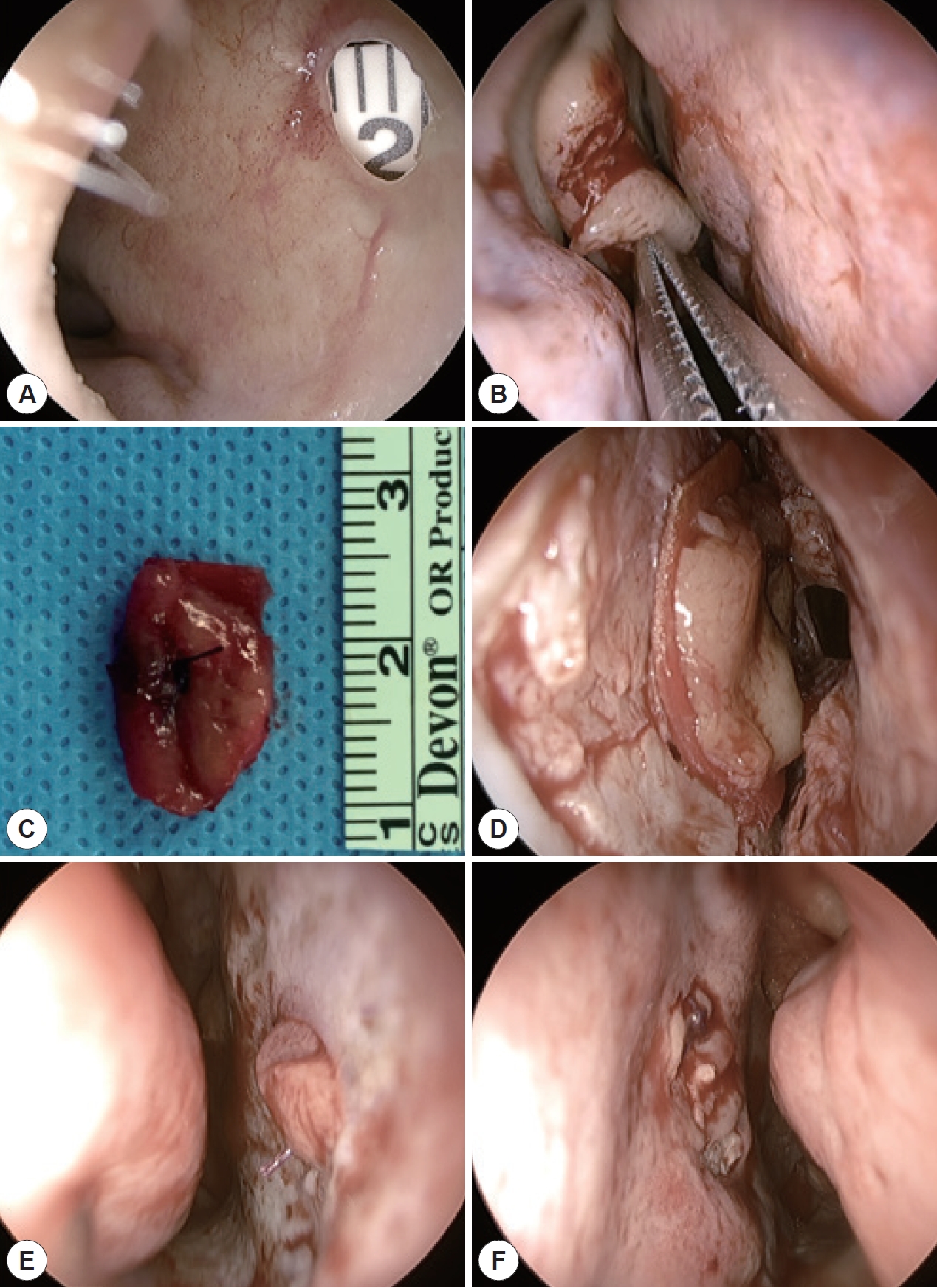
Fig.┬Ā2.
Illustration of endonasal septal perforation repair with free mucosal graft with Lyoplant® bioscaffold.

Fig.┬Ā3.
The preoperative and postoperative endoscopic views of septal perforation repair by free mucosal graft with Lyoplant® bioscaffold in 4 cases. A, D, G, J: Preoperative endoscopic view of nasal septal perforation (NSP) of enrolled patients. B, E, H, K: 2 weeks after the repair of NSP. C, F, I, L: Healed NSP at 3 months after surgery.

References
1) Hier MP, Yoskovitch A, Panje WR. Endoscopic repair of a nasal septal perforation. J Otolaryngol 2002;31(5):323ŌĆō6.


2) Lindemann J, Leiacker R, Stehmer V, Rettinger G, Keck T. Intranasal temperature and humidity profile in patients with nasal septal perforation before and after surgical closure. Clin Otolaryngol Allied Sci 2001;26(5):433ŌĆō7.


3) Goh AY, Hussain SS. Different surgical treatments for nasal septal perforation and their outcomes. J Laryngol Otol 2007;121(5):419ŌĆō26.


4) Mansour HA. Repair of nasal septal perforation using inferior turbinate graft. J Laryngol Otol 2011;125(5):474ŌĆō8.


5) Tastan E, Aydogan F, Aydin E, Can IH, Demirci M, Uzunkulaoglu H, et al. Inferior turbinate composite graft for repair of nasal septal perforation. Am J Rhinol Allergy 2012;26(3):237ŌĆō42.


6) Castelnuovo P, Ferreli F, Khodaei I, Palma P. Anterior ethmoidal artery septal flap for the management of septal perforation. Arch Facial Plast Surg 2011;13(6):411ŌĆō4.


7) Vuyk HD, Versluis RJ. The inferior turbinate flap for closure of septal perforations. Clin Otolaryngol Allied Sci 1988;13(1):53ŌĆō7.


8) Diamantopoulos II, Jones NS. The investigation of nasal septal perforations and ulcers. J Laryngol Otol 2001;115(7):541ŌĆō4.


9) Mobley SR, Boyd JB, Astor FC. Repair of a large septal perforation with a radial forearm free flap: brief report of a case. Ear Nose Throat J 2001;80(8):512.


10) Ayshford CA, Shykhon M, Uppal HS, Wake M. Endoscopic repair of nasal septal perforation with acellular human dermal allograft and an inferior turbinate flap. Clin Otolaryngol Allied Sci 2003;28(1):29ŌĆō33.


11) Kim SW, Rhee CS. Nasal septal perforation repair: predictive factors and systematic review of the literature. Curr Opin Otolaryngol Head Neck Surg 2012;20(1):58ŌĆō65.

12) Murrell GL, Karakla DW, Messa A. Free flap repair of septal perforation. Plast Reconstr Surg 1998;102(3):818ŌĆō21.


13) Kridel RW, Foda H, Lunde KC. Septal perforation repair with acellular human dermal allograft. Arch Otolaryngol Head Neck Surg 1998;124(1):73ŌĆō8.




 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Print
Print




